Adenosylmethionine is a potential agent in the treatment of ALD, and its mechanism is worth further investigation.
Alcoholic liver disease (ALD) is a series of liver diseases caused by long-term heavy alcohol consumption. In the course of its pathogenesis, a variety of complex pathophysiological mechanisms are involved.
Intestinal flora and endotoxin changes in alcoholic liver disease
Changes in intestinal flora and increased endotoxin permeability Alcohol increases intestinal permeability to endotoxins by changing intestinal flora.
Under normal circumstances, the gut flora is in a relatively stable equilibrium, and together with the intestinal mucosa, they form a barrier to prevent harmful substances such as endotoxins from entering the blood circulation.
Alcohol intake disrupts this balance, leading to changes in the intestinal flora that impair the barrier function of the intestinal mucosa and make it easier for endotoxins to cross the intestinal mucosa and enter the bloodstream.
At the same time as hyperendotoxemia, alcohol also reduces the intestinal ability to clear endotoxins.
This may be due to the damage of alcohol to intestinal mucosal cells, affecting their normal metabolism and function, including the uptake of endotoxins and metabolic capacity.
Endotoxin builds up in the blood, leading to hyperendotoxemia. Hyperendotoxemia is an important link in the pathogenesis of alcoholic liver disease, which can lead to a series of inflammatory reactions and pathological changes.
Changes in inflammatory cytokines
Hyperendotoxemia activates Kupffer cells to release TNF-α, TGF-β, IL-1, IL-6, IL-8 and other inflammatory cytokines.
These inflammatory cytokines trigger an inflammatory response in the liver, further damaging liver cells.
Levels of the protective IL-10 are down-regulated.
IL-10 is an anti-inflammatory cytokine that inhibits inflammation and protects liver cells.
When IL-10 levels drop, the liver is more vulnerable to damage from inflammation.
Mechanism of action of adenosylmethionine
Reducing TNF-α level and down-regulating the expression of TGF-β adenosylmethionine can decrease the level of TNF-α and down-regulate the expression of TGF-β.
TNF-α and TGF-β are two important inflammatory cytokines that play a key role in liver inflammation and fibrosis.
By reducing their levels and expression, adenosylmethionine is able to reduce the inflammatory response of the liver and slow the progression of liver fibrosis.
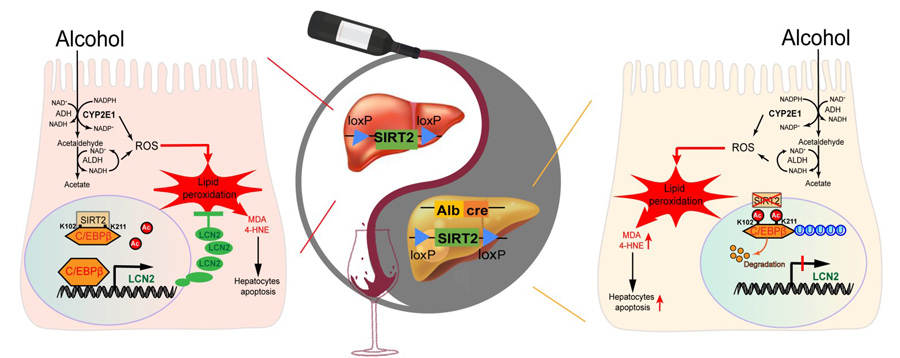
Inhibition of hepatocyte apoptosis and activation of adenosylmethionine by hepatic stellate cells also inhibited hepatocyte apoptosis and activation of hepatic stellate cells.
Hepatocyte apoptosis can reduce the number of liver cells and affect the normal function of the liver.
When activated, hepatic stellate cells transformed into myofibroblasts, which secrete a large amount of extracellular matrix and promote liver fibrosis.
Adenosylmethionine protects liver cells and prevents liver fibrosis by inhibiting these two processes.

Modulating the intracellular adenosylmethionine/S-adenosylcysteine ratio Adenosylmethionine can increase the intracellular adenosylmethionine/S-adenosylcysteine ratio and remove the increased S-adenosylcysteine in the cell.
The regulation of this ratio is important for maintaining the metabolic balance within the cell.
An increase in S-adenosine-cysteine may lead to an increase in oxidative stress responses within cells, affecting normal cell function.
Adenosylmethionine regulates this ratio to reduce oxidative stress in cells and protect liver cells.
Improving the liver microsomal glutathione reserve Adenosylmethionine can also improve the liver microsomal glutathione reserve.
Glutathione is an important antioxidant that protects liver cells from damage caused by free radicals.
By increasing the glutathione reserve, adenosylmethionine enhances the antioxidant capacity of the liver, prevents the occurrence of alcoholic liver damage, and delays the occurrence and development of liver fibrosis.
Sum up
Adenosylmethionine plays a role in alcoholic liver disease through a variety of mechanisms, including regulation of inflammatory cytokine levels, inhibition of hepatocyte apoptosis and hepatic stellate cell activation, regulation of intracellular metabolic ratios, and enhancement of antioxidant capacity.
These mechanisms help us to better understand the potential value of adenosylmethionine in the treatment of ALD,
and provide a theoretical basis for further research and clinical application.